In recent years, the world has faced numerous public health crises, from the COVID-19 pandemic to outbreaks of diseases in various regions. Now, another virus has risen to the forefront of global health concerns: mpox. Previously known as monkeypox, the World Health Organization (WHO) officially declared mpox a global public health emergency, triggering international action and awareness. This declaration not only highlights the severity of the outbreak but also the urgent need for coordinated efforts to control its spread and mitigate its impact.
In this 800-word overview, we’ll delve into the context, causes, and implications of WHO’s decision to label mpox as a global public health emergency, as well as the efforts underway to contain the virus.

What is Mpox?
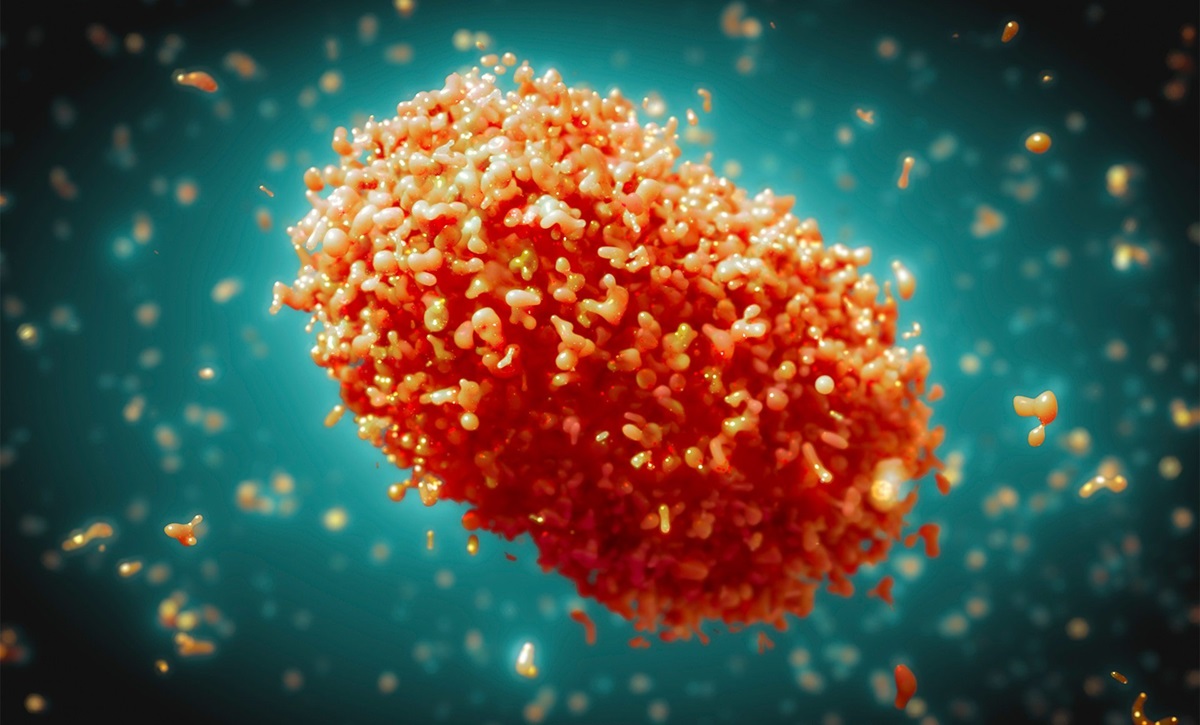
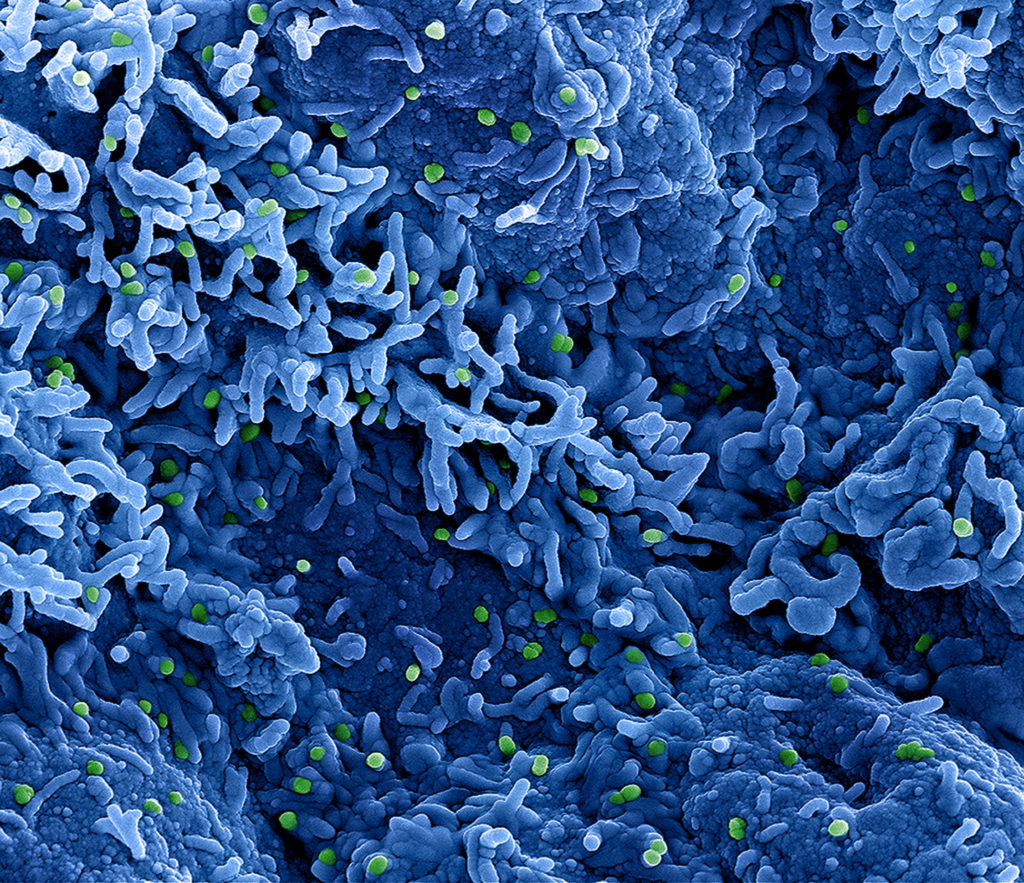
Mpox is a viral disease caused by the monkeypox virus, which belongs to the same family as the variola virus, the causative agent of smallpox. Despite their similarities, mpox is less deadly than smallpox, but it can still lead to serious health complications. Mpox was first discovered in 1958 among laboratory monkeys, hence its original name, although its primary transmission occurs through rodents and other wild animals.
Human cases of mpox were first identified in 1970 in the Democratic Republic of Congo (DRC), and since then, sporadic outbreaks have occurred, mainly in Central and West Africa. Mpox has long been endemic in several African countries, but until recently, it was largely unknown to the general public. This changed with the 2022-2023 outbreaks, which saw mpox cases rise dramatically in regions outside Africa, prompting widespread concern.
Symptoms and Transmission
Mpox typically presents with symptoms similar to those of smallpox, but generally milder. Common symptoms include:
- Fever
- Headaches
- Muscle aches
- Fatigue
- Swollen lymph nodes
- A distinctive rash that develops into fluid-filled pustules
The disease spreads primarily through close contact with an infected person, including contact with bodily fluids, skin lesions, or respiratory droplets. Transmission can also occur from handling contaminated objects, such as clothing or bedding, or through contact with infected animals. The virus enters the body through broken skin, respiratory tracts, or mucous membranes, such as the eyes, nose, or mouth.

Mpox has an incubation period of about 5 to 21 days, and while many people recover on their own within two to four weeks, vulnerable populations—such as children, pregnant women, and those with weakened immune systems—are at higher risk of severe illness or death.
The Global Outbreak and WHO’s Response
The current mpox outbreak, which began in early 2022, caught the world by surprise due to its spread in non-endemic regions. Countries across Europe, North America, and parts of Asia saw a rapid increase in mpox cases, often linked to international travel and community transmission. Unlike previous outbreaks, which were mostly confined to Africa, this global outbreak indicated that the virus had evolved to spread more efficiently among humans, sparking concern within the international health community.
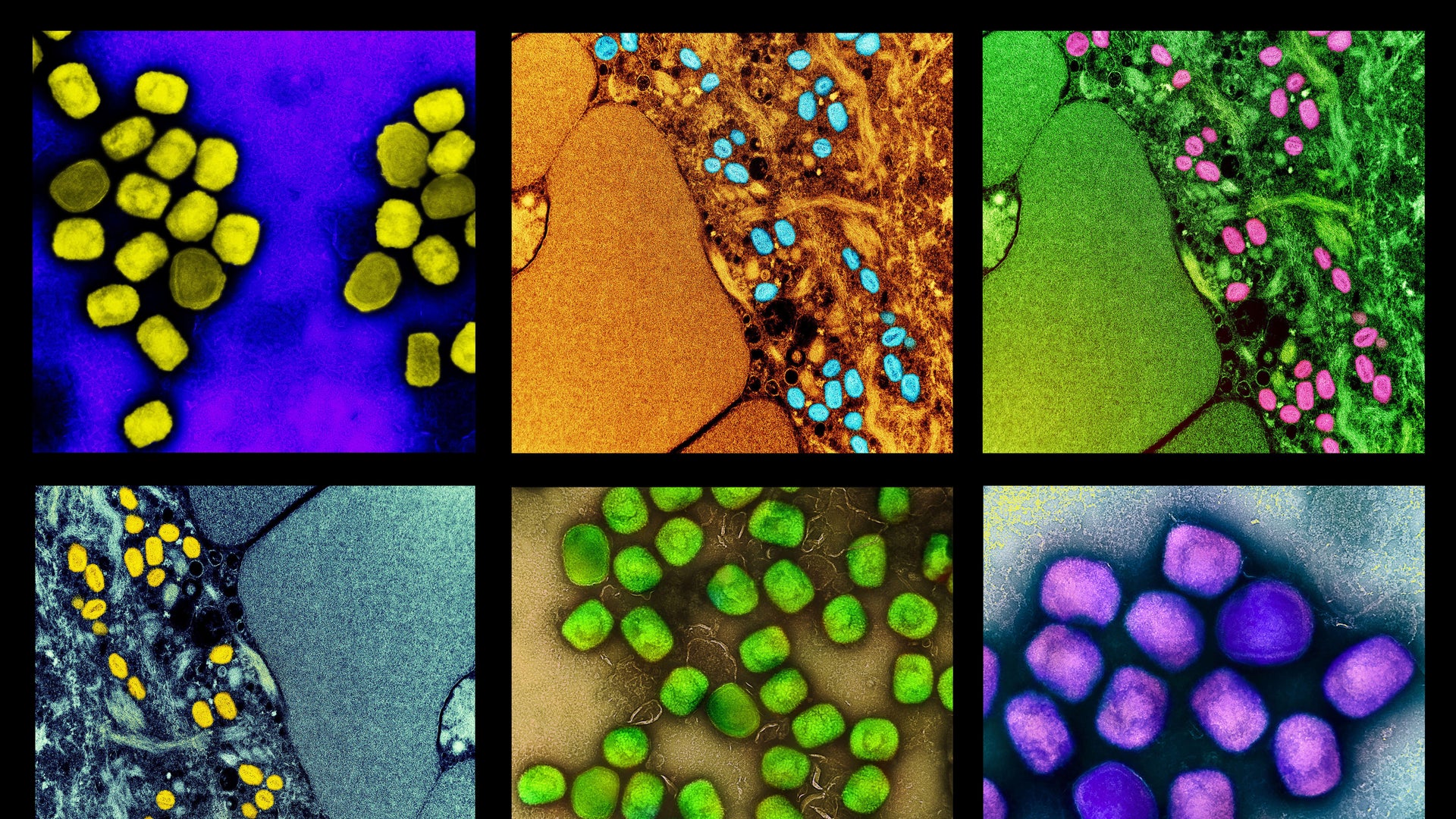
By mid-2023, mpox had spread to more than 75 countries, with over 60,000 confirmed cases. The rapid rise in infections and the geographic expansion of the virus pushed WHO to take decisive action. On July 23, 2022, WHO Director-General Dr. Tedros Adhanom Ghebreyesus declared mpox a Public Health Emergency of International Concern (PHEIC)—the organization’s highest level of alert. This declaration was a critical step, signaling that mpox posed a significant threat to global health and required an urgent, coordinated international response.

Why Was Mpox Declared a Global Public Health Emergency?
The decision to declare mpox a global public health emergency was driven by several factors:
-
Global Spread: Mpox, which was once confined primarily to Central and West Africa, had suddenly become a global concern. The virus rapidly spread across Europe, the Americas, and other regions, with little warning. The speed and scope of transmission were alarming, especially since many countries had never before dealt with mpox outbreaks.
-
Public Health Infrastructure: Many countries, particularly those outside Africa, lacked the infrastructure or experience to respond effectively to mpox. With health systems still recovering from the COVID-19 pandemic, the sudden outbreak of another infectious disease posed a significant challenge.
-
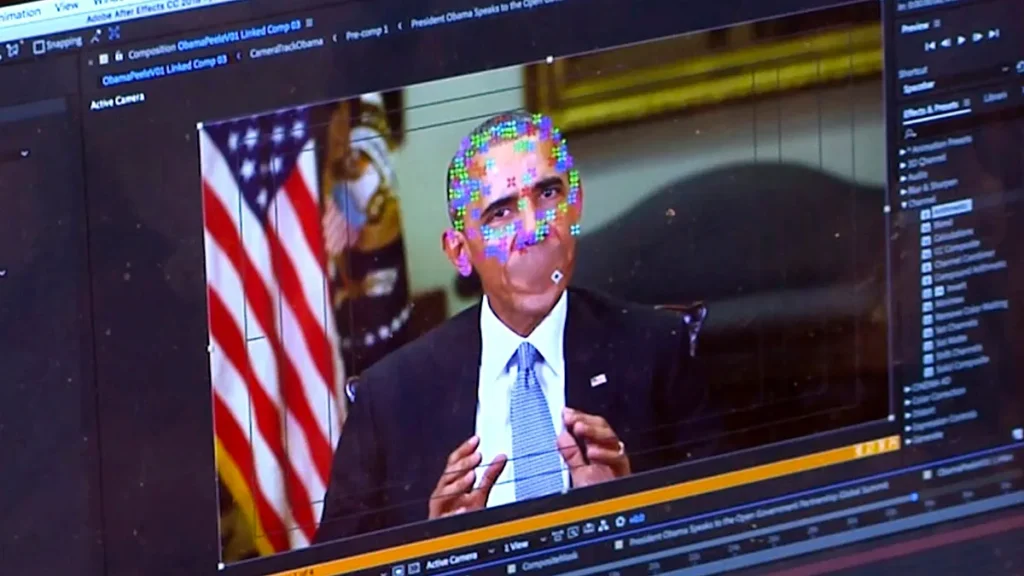
Stigma and Misinformation: Like many viral outbreaks, mpox was met with misinformation and stigma, particularly against certain communities. Early outbreaks were disproportionately affecting men who have sex with men (MSM), leading to stigmatization and fears of discrimination. WHO’s declaration emphasized the need for a compassionate, non-discriminatory response to avoid exacerbating stigma while ensuring that accurate information reaches the public.
-
Lack of Vaccination and Treatment: While smallpox vaccines are known to offer protection against mpox, most countries had stopped vaccinating their populations against smallpox after its eradication in the late 20th century. This left large portions of the global population susceptible to the virus. Additionally, antiviral treatments for mpox were limited, and there was an urgent need to ramp up vaccine production and distribution.
Global Response and Mitigation Efforts
WHO’s declaration of mpox as a global public health emergency has triggered a flurry of international efforts aimed at containing the outbreak and preventing further spread. Key measures include: